Twin to Twin Transfusion Syndrome Management
Not all families will choose one of these options. Some families feel the risks to mother mean they should not consider invasive treatment of any kind. Even in that case, our experienced team can help with critical management decisions.
A second option is to try and manage the symptoms of TTTS, but not actually treat the condition. Although our team has years of experience with those procedures, we now believe they should be used only in very specific limited circumstances.
The advances of ultrasound assessment and minimally invasive intrauterine surgery mean that our team, directed by Dr. Christopher Harman, can offer several definitive options for the treatment of TTTS.
Non-Invasive Management
Medications, given orally or intravenously, can be used to modify the fetuses' circulations, the recipient's amniotic fluid production and preterm labor. Many of these cross the placenta and can have very serious side-effects on both fetuses and mother.
Symptomatic Management
Amniocentesis/Amniodrainage
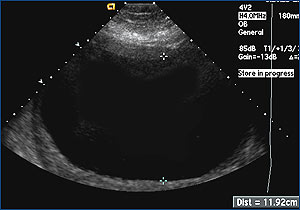
The procedure of amniodrainage/septostomy involves draining the excess amniotic fluid. Using ultrasound guidance, a needle is positioned in the recipient's sac and 2-3 liters of fluid are gently removed. This therapy aims at preventing the risk of preterm delivery from over-distension of the uterus. Because the underlying cause of TTTS continues, the fluid in the sac re-accumulates. Therefore, amniodrainage may need to be repeated multiple times over the course of a pregnancy.
Amniocentesis may be combined with a "septostomy". In this procedure, fluid is first drained from the amniotic sac and then the needle is used to make a small hole in the membrane between the twins' two amniotic cavities. This allows amniotic fluid to pass into the sac of the donor twin. Recent studies have shown that a septostomy does not produce any improved outcomes over amniodrainage alone.
Amniotic fluid manipulation, such as with amniodrainage or septostomy, may relieve symptoms and may ease the problems of TTTS in some patients. However, since the anastomoses remain open, the risks of unbalanced volume exchange also remain - the underlying problem is not "fixed".
The outcomes with serial amniodrainage reported in the literature vary widely. Two twins may survive in up to 42%, one twin in 18% and in 40% of cases both twins are lost. In addition a 20 % risk of variable neurological damage ("brain damage") remains for the surviving babies.
Procedures for Definitive Treatment
Umbilical Cord Occlusion: This procedure is done inside the uterus, through a sheath placed by ultrasound guidance in the sac of one twin, usually the donor (smaller) twin. Special tweezers grasp the cord and an electric current passes between the jaws of the tweezers, coagulating the blood vessels of that twin's cord. This stops the flow of blood in the cord and that baby dies.
The surviving baby usually has no long-term effects. As with any intrauterine invasive procedure, there can be short-term complications, including preterm labor, rupture of membranes, infection or bleeding. But, in more than 90% of cases, the procedure results in one living baby, born near term, with no permanent handicaps. For an experienced team, this procedure is technically feasible and usually not long, so maternal operative complications are very unusual.
Because the umbilical cord is completely blocked, this procedure means survival of both babies can never occur. This procedure may be the best if one twin seems to have damage or abnormalities already, or has IUGR too severe for survival.
Laser Ablation
Laser ablation of placental anastomoses was pioneered in the US and has been performed for over ten years in North America and Europe. The procedure aims to treat the underlying cause of TTTS by coagulating vascular anastomoses with a laser beam. Under initial ultrasound guidance, a tiny camera is inserted through a fetoscope (a thin, flexible instrument) into the uterus. Once inserted, direct vision through the fetoscope is used first to identify the connecting vessels and second to coagulate or seal them shut. Coagulating the vessels stops the blood flow between the donor and recipient through the placenta. The coagulation is done on the surface of the placenta, in the territory between the twins, where the imbalanced blood volume sharing takes place. The umbilical cords themselves are not interfered with.
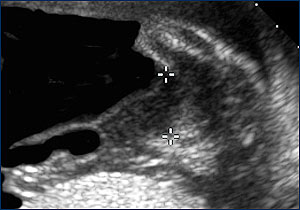
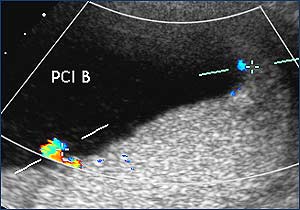
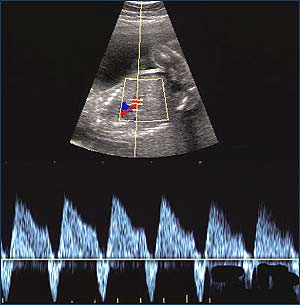
Ultrasound is used to identify the placental cord insertion of each baby (colored points).
An advantage of this therapy is treatment of the underlying cause with a single procedure. Following the closure, both twins have a chance for subsequent normal development. As with any invasive procedure, there are risks associated with the outcome.
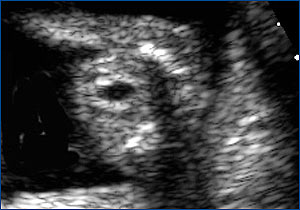
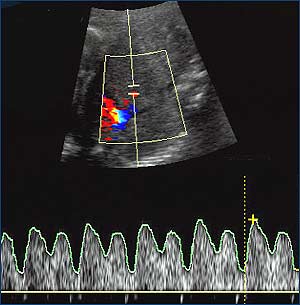
After successful treatment, the donor bladder begins to fill (small black circle in the middle of the abdomen) and the blood flow in the umbilical cord improves (right image).
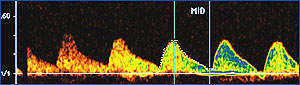
On the recipient side, there is gradual improvement in heart failure from the abnormal tracing before the laser treatment (part of the blood flow in the heart cycle runs backwards, on the left) to normal cardiac function with all blood flow forward (on the right).
To date, approximately 1,000 procedures have been performed in five major European centers as part of a collaborative trial (Eurofetus project). Results published after the first 220 procedures show the chance for survival of both twins is 55%, survival of at least one twin is 82% and the risk for loss of both twins is 18%. Some increased risk for neurological damage in surviving babies remains, but is significantly lower than the risk following serial amnioreduction (less than 9%). More results are now being reported, with even more reassuring outcome.
While there are problems with laser ablation, it remains the best chance of having two healthy surviving babies delivered near term.
Choosing the Right Management Plan
Choosing the management option most appropriate for you is a challenging task. As parents, your choice is very individual and there is no "right" or "wrong" decision. It is important to consider all of your options before making a management decision. For example, an initial amnioreduction removes the necessary amniotic fluid pocket for successful laser therapy and may, therefore, limit or delay the possibility for definitive treatment. The following table gives you an overview of the typical procedure-related risks and outcomes.
Acute previable TTTS management options and outcome
Acute Previable TTTS Management Options and Outcome
| Management Plan | Both Survive | One Survives | Brain Injury | Both Die | Procedural Risk |
|---|---|---|---|---|---|
| Do nothing, observe | <5% | <30% | 50% | 70% | 2-5% M |
| Pregnancy termination | 0 | 0 | - | 100% | 1-2% M |
| Serial amniodrainage | 42% | 60% | 20% | 40% | 4% F, procedure |
| Umbilical cord ligation | 0 | 95% | 4-6% | 5% | 10% F, 1-2% M |
| Laser coagulation | 60% | 82% | 10% | 18% | 10% F, 1-2% M |
F = fetal; M = maternal
