Resident Training Program - Internal Medicine Residency
The education and clinical training of Internal Medicine residents is a central focus in the Department of Medicine. We provide comprehensive training in general internal medicine for residents seeking career in a subspecialty fellowship, primary care and hospital medicine.
Combined training programs in Medicine-Pediatrics and Internal Medicine-Emergency Medicine (including a 6th year for EMIM-Critical Care certification) offer unique opportunities to individuals interested in dual or triple certification.
Our broad and flexible curriculum allows residents to individualize a well-rounded program suitable for their personal educational needs. Residents participate in a comprehensive core curriculum that emphasizes the breadth and depth of internal medicine and a broad choice of electives that allow them to explore areas of clinical and research interest.
Goals of the Residency Education Program
Through their clinical training, residents:
- Learn the principles and knowledge necessary for the practice of general internal medicine balanced with a comprehensive exposure to the medical subspecialties.
- Gain clinical knowledge in diverse ambulatory and inpatient settings by caring for patients with a variety of illnesses and from many socioeconomic backgrounds.
- Receive a balanced exposure to patients with acute or life threatening illnesses and to those with chronic or subacute problems.
- Are immersed in a clinical learning environment that promotes wellness and supports a healthy work-life balance.
- Engage in a supportive community that addresses issues related to bias, anti-racism, community engagement.
To meet these goals, residents gain clinical experience at three teaching hospitals and numerous ambulatory sites. Residency training is conducted at the University of Maryland Medical Center, Veterans Affairs Medical Center and Mercy Medical Center -- a community hospital within five minutes from University Center. Training in ambulatory care takes place at these sites and in clinics and private practices in Baltimore City and surrounding counties.
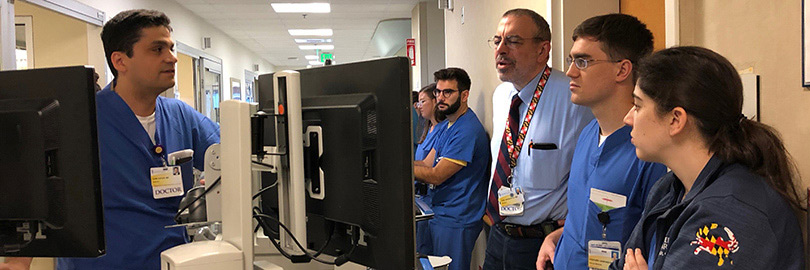
The Clinical Learning Environment
We are deeply committed to ensuring our residents learn in a supportive environment that emphasizes clinical medicine, individualized mentoring and resident wellness.
Here are some highlights of our clinical curriculum and structure:
- General medicine teams
- UMMC teams, include 1 attending, 1 senior resident + 2-3 interns in a daytime admitting structure. Our AIR team (Admitting Intern and Resident) admit patients to the GIM teams at UMMC and the Night Float Team covers 7 nights/week. Resident moonlighters provide cross-coverage for the teams from 5-9PM on weekdays.
- VA teams, include 1 attending 1 senior resident + 2 interns in a team call structure. Day Float residents assist the general medicine teams with admissions. A night float team cover 7 nights/week.
- To ensure compliance with work hour rules, residents have caps on the number of admissions per shift and during the last few hours of their shift.
- Patient care in the ICUs is always a team approach - with residents, fellows and intensivists on site 24/7/365.
- Our cardiology services have continuous cardiology fellow support.
- Call on all services at all sites - including floor teams and ICU's is every fourth day.
- We track resident work hours through a self-reporting method to ensure compliance with all ACGME Duty Hour Requirements.
- Interns are strictly capped at 5 admissions with upper-level residents capped at 10 supervisory admissions.
- Interdisciplinary teams and discharge planners facilitate patient care. Broad ancillary services at all sites make patient care efficient and effective.
- All sites have full electronic medical records, with EPIC at UMMC and Mercy, and CPRS at the VA.
- Non-teaching services admit patients at all sites to help patient flow and ensure we meet all ACGME rules. At UMMC, we have non-teaching services for general medicine, step-down intermediate care unit (IMC), BMT, solid organ transplant services and bone marrow transplant unit. The VA and Mercy have general medicine nonteaching services.
Leadership and Teaching Skills
The development of leadership and teaching skills is an important part of residency training. Throughout their rotations, residents develop the necessary skills to be clinical supervisors and teachers of the medical teams. By taking on progressive responsibilities, residents become comfortable dealing with a wide variety of clinical situations, including patient care, interpersonal situations and teaching.
Residents attend annual educational retreats where they improve their skills in giving feedback, teaching in small groups, managing conflict, and team building. An educational retreat for interns in the fall helps to boost their skills early in the year and provides a dinner social event to enjoy time with their classmates. A best resident-teacher award is given to a senior resident each year -- reaffirming the importance placed on excellence in teaching as part of each resident's core responsibilities.
Our residents consistently receive the majority of the teaching awards given by the medical students, including AOA Honor Society and the Gold Humanism Honor Society. The strength of our residents' student teaching is one of the main reasons that our Internal Medicine Clerkship is ranked as one of the best in the country!



