Lumbar Interbody Fusion
A Patient's Guide to Anterior Lumbar Interbody Fusion
Introduction
The vast majority of patients who have low back pain will not need surgery to treat their condition. However, sometimes surgery can help when all other methods have failed to bring relief. Many very different problems can cause low back pain. No one type of surgery is right for the treatment of every problem that causes low back pain.
Spinal fusion has been used for many years to treat many painful conditions in the lumbar (lower) spine. Over the past decade, there has been dramatic improvement in the way that spinal fusion operations are performed. One major improvement has been the development of fixation devices. Designed to stabilize and hold the bones together while the fusion heals, these devices have greatly improved the success rate of fusion in the lower back.
This document will discuss:
- The lumbar spine anatomy
- The rationale of the operation
- The way the operation is performed
- Some of the devices that are used
- The use of bone graft
- What to expect during your rehabilitation
- Some of the possible complications
Anatomy
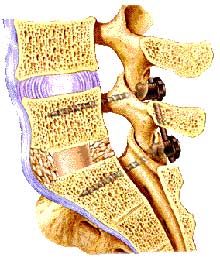
To better understand how a lumbar spinal fusion is performed, it is helpful to know some anatomy of the spine and more specifically, the parts of the spine involved in the surgery: the lumbar spine, pedicles, nerve roots, and laminae.
Please review the document, entitled:
Rationale of the Operation
One of the main goals of any surgical procedure on the skeletal system is to stop the pain caused by joints that have worn out over time - joints that are degenerative. One of the most reliable ways to reduce pain from degeneration of any joint is to fuse that joint together. A fusion is an operation where two bones, usually separated by a joint, are allowed to grow together or fuse into one bone. This is true in the spine as well. A fusion is also sometimes called an arthrodesis of the joint.
Several back conditions may lead to the need for a spinal fusion. Your spine specialist may suggest a spinal fusion if all other conservative treatments have failed for the following conditions:
Degenerative Disc Disease
Degeneration, or wear and tear of the discs between one or more vertebrae can lead to a painful condition that may require a spinal fusion of the vertebrae on both sides of the degenerative disc. The intervertebral discs are flat, round "cushions" that act as shock absorber between each vertebra in your spine. The disc allows motion to occur between each vertebra. Removing a degenerated disc and allowing the two vertebrae to grow together or fuse can reduce the pain from the condition.
If you would like further information about degenerative disc disease, you may wish to review the document, entitled:
Instability of the Spine
Each spinal segment is like a well-tuned part of a machine. All of the parts should work together to allow weight bearing, movement, and support. Remember that a spinal segment is composed of two vertebrae attached together by ligaments, with a soft disc separating them. The facet joints fit between the two vertebrae, allowing for movement, and the foramen between the vertebrae allows space for the nerve roots to travel freely from the spinal cord to the body. When all the parts are functioning properly, the spinal segments join to make up a remarkably strong structure called the spine. When one segment deteriorates to the point of instability, it can lead to localized pain and difficulties.
Segmental instability occurs when there is too much movement between two vertebrae. The excess movement of the vertebrae can cause pinching or irritation of nerve roots. It can also cause too much pressure on the facet joints, leading to inflammation of facet joints. It also may cause muscle spasms as the paraspinal muscles try to stop the spinal segment from moving too much. The instability eventually results in faster degeneration of the spine in this area.
Adult Scoliosis
Scoliosis is a condition where the spine has an abnormal curve when viewed front to back. Scoliosis can be the result of many different conditions and the treatment of each is very different. The type of scoliosis this document refers to is adult scoliosis. The treatment is much different than the type of scoliosis teenagers develop, or the type of scoliosis children may be born with.
Sometimes in an adult, the curve is simply a result of poor posture or back muscle spasms. However, sometimes the curve is actually due to the spine itself being abnormal. Scoliosis can also develop over many years from a neurological disorder like muscular dystrophy. In adults, scoliosis may result from degeneration of the spine in old age that leads to the deformity.
If you would like further information about Adult Scoliosis of the Spine, you may wish to review the document, entitled:
Spondylolysis/Spondylolisthesis
Spondylolysis refers to a defect in one of the vertebra in the lower back, generally the last vertebra of the lumbar spine. The area of the vertebra called the pedicle is affected. The pedicle is part of the bony ring that protects the spinal nerves. The pedicle also connects the vertebral body to the facet joints. When a spondylolysis is present, the back part of the vertebra and the facet joints simply are not connected to the body - except by soft tissue.
Spondylolisthesis is the term used to describe when one vertebra slips forward on the one below it. This usually occurs because there is a spondylolysis in the vertebra on top. There are two main parts of the spine that keep the vertebrae aligned - the disc and the facet joints. When a spondylolysis occurs, the facet joint can no longer hold the vertebra back. The intervertebral disc may slowly stretch under the increased stress and allow the upper vertebra to slide forward.
If you would like further information about spondylolysis and spondylolisthesis, you may wish to review the document, entitled:
Devices Used in Lumbar Spine Fusion
In the past, spinal fusions of the lumbar spine were performed without any internal fixation. The surgeon simply roughed up the bone, placed bone graft material around the vertebrae, and hoped the bones would fuse. Sometimes, patients were placed in a body cast to try to hold the vertebrae somewhat still while healing took place. The patient was lucky to have a 70% chance of successful fusion.
Today, there are many different types of metal devices used to perform a lumbar fusion. These devices connect two or more vertebrae together, hold them in the correct position, and keep them from moving until they have a chance to grow together, or fuse. This is not an easy task. The vertebrae are small, so there is not much room to put in the screws, plates, or metal rods that surgeons typically use to connect bones. Another problem is that many nerves get in the way of putting screws into the vertebral body. Finally, there is a great deal of stress across the lumbar spine when standing upright or even sitting. Finding a metal device that is able to hold the bones together can be difficult.
Over the past two decades, some very ingenious devices have been designed. They have changed the way surgeons perform spinal fusions. Most of the current devices that surgeons favor use metal screws that are placed through the small tube of bone, called the pedicle, and into the vertebral body. These screws are attached to metal plates or metal rods that are bolted together in the back of the spine. This combination of hardware creates a solid "brace" that holds the vertebrae in place. These devices are intended to stop movement from occurring between the vertebrae that are being fused, allowing a solid fusion to occur. These metal devices give more stability to the fusion site and allow the patient to be out of bed much sooner.
The Operation
There are two main types of spinal fusions: a posterior approach and an anterior approach.
Posterior Approach
The posterior approach is done from the back of the patient and can either just fuse the vertebral bones or include removal of the problem disc. If the disc is removed, it is replaced with a bone graft. This is called a posterior lumbar interbody fusion.
With a posterior approach, an incision is made in the middle of the lower back over the area of the spine that is going to be fused. The muscles are moved to the side so that the surgeon can see the backside of the vertebrae.
Once the spine is visible, the lamina of the vertebra is removed to take pressure off the dura and nerve roots. This allows the surgeon to see areas of pressure on the nerve roots caused by bone spurs, a bulging disc, or thickening of the ligaments. The surgeon can remove or trim these structures to relieve the pressure on the nerves. Once the surgeon is satisfied that all pressure has been removed from the nerves, a fusion is performed.
When operating from the backside of the spine, the most common method of performing a spinal fusion is to place the bone graft around the back side of the vertebrae. Today, the surgeon will also most likely use some type of metal screws, plates, and rods to hold the vertebrae in place while the spine fusion heals. Special screws called pedicle screws are inserted into the vertebral body. These screws are placed down the small bony tube created by the pedicle on each side of the vertebra, between the nerve roots. This allows the screws to grab into the bone of the vertebral body, giving them a good solid hold on the vertebra. Once these screws are placed, one in each pedicle, they are attached to metal rods that connect all the screws together. Once everything is bolted together and tightened, this creates a stiff metal frame that is intended to hold the vertebrae still so that healing can occur. Finally, bone graft is placed around the back of the vertebrae. The bone graft helps the vertebrae heal together, or fuse.
To learn more about what bone graft is and how it is used, please review the document, entitled:
Anterior Approach
In some cases, it may be better to consider placing the bone graft between the vertebral bodies. The anterior approach (meaning from the front) allows the surgeon to remove the intervertebral disc from the front and place the bone graft between the vertebrae. This type of operation is usually done by making an incision in the abdomen, just above the pelvic bone. The organs in the abdomen, such as the intestines, kidneys, and blood vessels are moved to the side. This allows the surgeon to see the front of the spine.
The surgeon then determines which intervertebral disc is the correct one and removes it. Bone graft is then placed into the area between the vertebrae where the disc has been removed. Recently, surgeons have begun using implants that are designed to spread the two vertebrae and hold them apart while the fusion heals. These implants are made from various materials including metal, bone, coral, and now graphite fiber.
For more information concerning this type of fusion, you may wish to review the document entitled:
Combined Anterior and Posterior Approach
When performing a spinal fusion from the posterior approach (the back side), it is possible to move the spinal nerves to the side and place bone graft in between the vertebral bodies themselves. This is sometimes referred to as a "posterior lumbar interbody fusion" (PLIF). Today, surgeons are also beginning to place intervertebral cages between the vertebral bodies to hold the two vertebrae apart as the fusion heals. In some cases, this can be done from the back side of the spine without the necessity of making an additional incision in the patient's abdomen (from the front).
Working between the vertebrae from the back side has limitations. The surgeon is limited by the fact that the spinal nerves are constantly in the way. These nerves can only be moved a slight amount to either side. This limits the ability of the surgeon to see the area. There is also limited room to use instruments and place implants between the vertebrae. For these reasons, many surgeons prefer to make a separate incision in the abdomen and actually perform two operations - one from the front of the spine to perform an anterior spinal fusion and one from the back to perform a posterior fusion. The two operations are usually done at the same time; however, this is not necessary. They may be done several days apart.
Rehabilitation
Because it takes about three months for fusions to mature and become solid, it is vital that you avoid any activities that could harm the bone graft. The bone graft will continue to heal and become stronger over the following couple of years. After surgery, all of your muscles will be much weaker, so an appropriate exercise program will need to be developed to get you and your back into optimal condition. Rehabilitation will focus on: strengthening the muscles, stretching for maximum flexibility, and aerobic exercise. A physical therapist will help you develop a program suited for your condition and needs. For a complete recovery, it is important to stick with your program.
For more information on general principles of rehabilitation, you may wish to review the document, entitled:
Complications
With any surgery, there is a risk of complications. When surgery is done near the spine and spinal cord, these complications (if they occur) can be very serious. Complications could involve subsequent pain and impairment and the need for additional surgery. You should discuss the complications associated with surgery with your doctor before surgery. The list of complications provided here is not intended to be a complete list of complications and is not a substitute for discussing the risks of surgery with your doctor. Only your doctor can evaluate your condition and inform you of the risks of any medical treatment he or she may recommend.
Please review the document, entitled:
Copyright © 2003 DePuy Acromed.
